Watch this week's FLCCC webinar, 'Managing Type 2 Diabetes: Simple Steps to Better Health', with Dr. @joevaron and Dr. @kristina_carman, here.
— FLCCC Alliance (@Honest_Medicine) September 19, 2024
'Type 2 Diabetes Is Surging—Can It Be Reversed?' Read new post: https://t.co/Wxggi6qBI5
Read and download new 'Blood Sugar Hacks'… pic.twitter.com/XGbASSjuQt
Speakers: Dr. Joseph Varon, Dr. Kristina Carman
“Let food be thy medicine, and let medicine be thy food.” – Hippocrates
Type 2 Diabetes is more than just a chronic condition—it’s an accelerator and driver of mortality worldwide. According to the World Health Organization, more than 420 million people globally are living with diabetes, and about 90% of them have Type 2 Diabetes. In the United States alone, more than 37 million people have diabetes, with Type 2 Diabetes being the most common form. It’s not just about high blood sugar levels; unmanaged Type 2 Diabetes can lead to serious health complications like heart disease, stroke, kidney failure, and blindness.
Living with Type 2 Diabetes can feel overwhelming and isolating. The daily challenges of managing blood sugar levels, the fear of complications, and the lifestyle adjustments can take a toll. But you’re not alone, and there is hope. By understanding how your body works and making simple lifestyle changes, you can take control of your health.
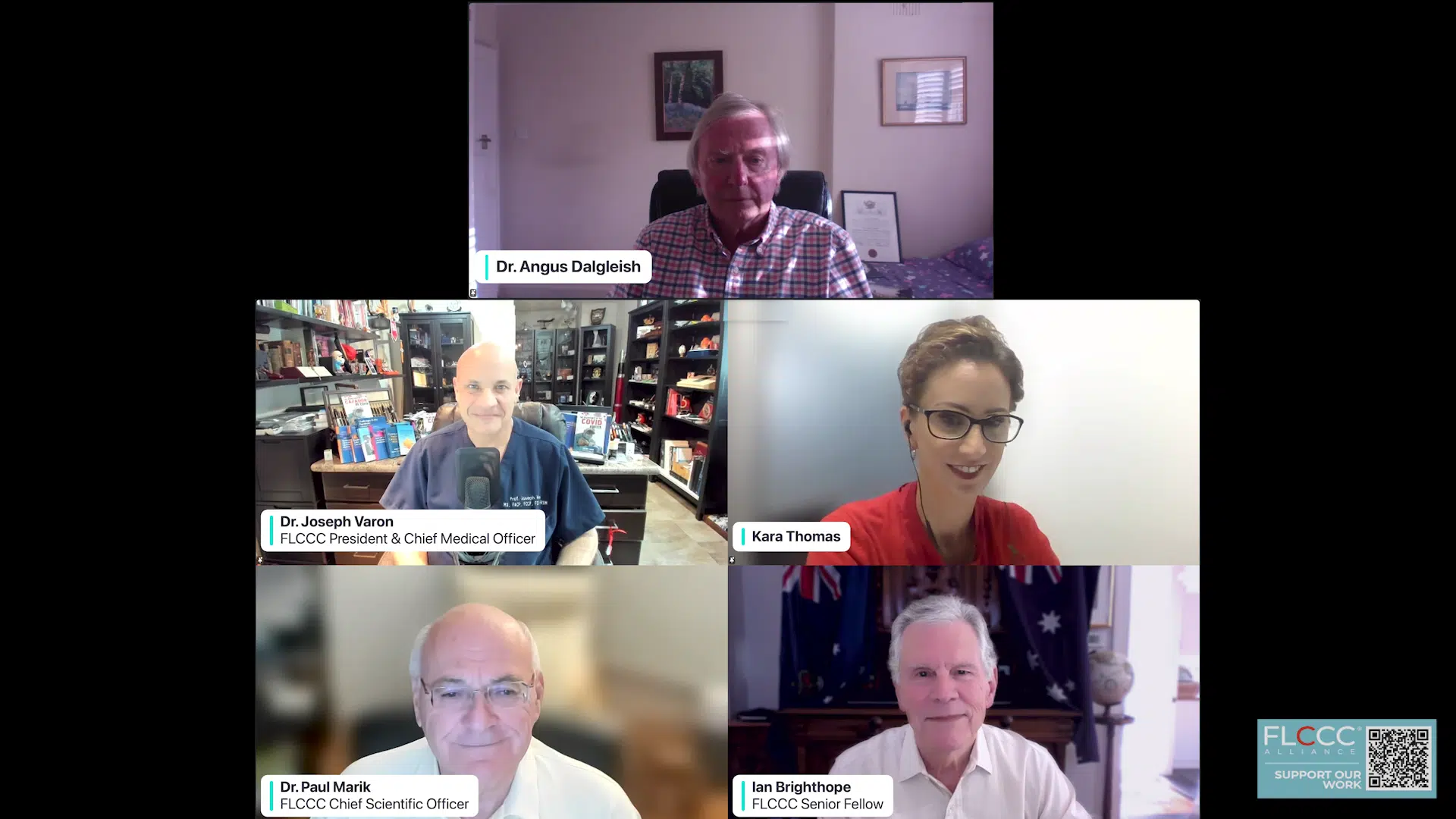
In this webinar, we are treated to insights from two outstanding medical professionals: FLCCC President Dr. Joseph Varon, and FLCCC Senior Fellow Dr. Kristina Carman. Together, they will explore the many ways people with type 2 diabetes can manage their condition.
As we’ll learn, managing diabetes does not mean taking 6 different medications every day! With relatively simple lifestyle adjustments, many patients can start to reverse type 2 diabetes. So, do not hesitate to press play on the video above or keep scrolling. If you or anybody you know needs diabetes care, you won’t want to miss this.
Understanding Type 2 Diabetes
Type 2 Diabetes, also known as adult-onset diabetes, is the most common form of diabetes mellitus. It occurs when the body becomes resistant to insulin or doesn’t make enough insulin to maintain normal blood sugar levels. Insulin is a hormone produced by the pancreas that allows glucose to enter cells to produce energy.
Symptoms and Causes
Recognizing the symptoms of Type 2 Diabetes is essential for early diagnosis and treatment. Early symptoms include:
- Increased thirst
- Frequent urination
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
Some people may not experience noticeable symptoms, making regular check-ups important.
Several factors can increase the risk of developing Type 2 Diabetes, including genetics, obesity, a sedentary lifestyle, and age. People with a family history of diabetes, those who are overweight, and individuals over the age of 45 are more likely to develop the condition.
👇 Struggling with Blood Sugar? Check out these blood sugar hacks from Dr. Carman!
The Role of Insulin and Glucose
When you eat, your body breaks down carbohydrates into glucose, raising your blood sugar levels. In response, the pancreas produces insulin to help cells absorb glucose. In Type 2 Diabetes, cells become resistant to insulin, or the pancreas doesn’t produce enough insulin, leading to high blood sugar levels.
The gastrointestinal tract plays a significant role in this process. The rate of gastric emptying—the speed at which food leaves the stomach—affects the glycemic response. Additionally, hormones like incretins influence insulin release and action.
Gastric emptying refers to the rate at which food leaves your stomach and enters the small intestine. This process significantly impacts blood sugar control because it determines how quickly glucose is absorbed into the bloodstream.
“The rate of emptying of your stomach is probably one of the major determinants of this response to insulin.” – Dr. Joseph Varon
A slower gastric emptying rate leads to a more gradual absorption of glucose, preventing sharp spikes in blood sugar levels. This allows insulin to work more effectively, aiding in better management of Type 2 Diabetes. Factors such as the type of food consumed, meal composition, and even stress levels can influence gastric emptying.
The Use of New Diabetes Treatments
Building on the concept of gastric emptying, certain medications have been developed to leverage this mechanism for better blood sugar control. One such class of drugs includes semaglutide, a GLP-1 receptor agonist.
“One reason why they seem effective is because they delay the gastric emptying.” – Dr. Joseph Varon
Semaglutide works by mimicking the action of the GLP-1 hormone, which not only stimulates insulin release but also slows gastric emptying. This dual action helps to lower blood sugar levels after meals and can contribute to weight loss by increasing feelings of fullness.
However, there’s a mixed consensus on the long-term use of these medications. While they can be effective in managing blood sugar levels, reliance on them without addressing lifestyle factors raises concerns.
“I do believe that some people need help to get them over a hump… What I do have a big issue with is, does that mean you have to be on these medications long term? Once you go on it, you’re on it forever, and that shouldn’t be the case.” – Dr. Kristina Carman
Dr. Carman emphasizes that while medications like semaglutide can provide immediate support, they shouldn’t replace foundational lifestyle changes such as diet modification and increased physical activity. She also raises concerns about the impact of these medications on gut health.
“My other issue when it comes to these types of medication is the effect it has on the microbiome, simply because we have GLP-1 antagonists within us already. And there are ways that we can signal and turn these on just by simple things that we’re doing through our diet and through our lifestyle and the way that we’re eating and the order of the way that we’re eating.” – Dr. Kristina Carman
The human gut microbiome plays a crucial role in overall health, including glucose metabolism and insulin sensitivity. Altering it with medications may have unintended consequences. Therefore, it’s essential to consider the potential long-term effects and to use such treatments as part of a comprehensive diabetes management plan that prioritizes natural methods whenever possible.
Simple Steps to Manage Type 2 Diabetes
In this webinar, the doctors left nothing on the table. People with diabetes will be happy to know that the suggestions below are all natural, safe, and healthy ways to manage type 2 diabetes. Here’s what’s on deck:
- Slow Down and Be Mindful When Eating
- Eat Early in the Day
- Incorporate Yogurt and Fermented Foods
- Utilize Natural Remedies
- Regular Physical Activity
- Prioritize Sleep and Stress Management
- Focus on Gut Health with Probiotics
- Incorporate Whole Grains, Nuts, and Seeds
- Consume Flavonoid-Rich Foods
1. Slow Down and Be Mindful When Eating
“If you slow it down and really mindfully chew your food, chew it so that it’s unrecognizable in your mouth, it can have a profound effect on your glucose spikes post-meal.”
Eating slowly and mindfully can have a profound effect on blood sugar levels. Dr. Carman emphasizes that if you take the time to chew your food thoroughly it can significantly reduce glucose spikes after meals. And by avoiding distractions like television or smartphones during meals, you become more attuned to your body’s signals.
2. Eat Early in the Day
According to some studies, consuming larger meals earlier can improve glycemic control. Dr. Joseph Varon notes that eating early in the day can enhance body weight control and glycemic management. This approach reduces postprandial (after eating) blood sugar peaks and enhances insulin sensitivity. It also helps regulate hunger hormones, reducing appetite later in the day.
- Improves body weight control & glycemic control
- Lowers diabetes risk
- Decreases postprandial glucose peak
- Increases postprandial insulin (secretion/sensitivity), ↑GLP-1
- Improves ghrelin regulation
3. Incorporate Yogurt and Fermented Foods
“There have been a lot of randomized control trials that have shown that both yogurt and cheese may impact what your inflammatory markers show in your body. And again, these inflammatory markers go hand by hand with what happens to your blood sugar.”
Adding yogurt to your diet can help manage Type 2 Diabetes. According to Dr. Varon, consuming products like yogurt decreases inflammation, which in turn lowers sugar levels. Yogurt contains probiotics that improve gut health and reduce inflammation linked to insulin resistance. It’s also rich in essential nutrients like calcium and magnesium.
When choosing yogurt, opt for plain, unsweetened varieties with live cultures. Dr. Carman advises reading labels carefully to avoid added sugars and to ensure the presence of beneficial bacteria strains.
4. Utilize Natural Remedies
Cinnamon
Cinnamon has been traditionally used to help lower blood sugar levels. Dr. Varon highlights that cinnamon can improve insulin sensitivity and lower fasting blood sugar levels. Incorporating cinnamon into your diet is simple—you can add it to oatmeal, smoothies, or tea. However, consult your healthcare provider before taking cinnamon supplements.
“One of the best beautiful sort of digestive aids that we can sort of layer in, particularly if you tend to bloat after you eat, is some fresh ginger, some fennel seeds, and some cinnamon steeped in some hot water. It’s excellent, and it will really support that glucose tolerance and help digestion.”
Vinegar
Consuming vinegar before meals can reduce blood sugar spikes. Dr. Carman mentions that a little bit of vinegar can be supportive and helpful. Mixing one to two tablespoons of apple cider vinegar with water and drinking it before your largest meal can enhance insulin sensitivity and reduce postprandial blood sugar levels.
5. Regular Physical Activity
Exercise’s Impact on Blood Sugar
Physical activity helps lower blood sugar levels and improves insulin sensitivity. Dr. Varon emphasizes that even moderate exercise, such as 20 to 30 minutes of aerobic activity three times a week, can make a significant difference. Activities like walking, strength training, cycling, or swimming are effective. Including strength training exercises and staying active throughout the day also contribute to better blood sugar management.
6. Prioritize Sleep and Stress Management
The Role of Sleep
Sleep deprivation affects hormone secretion and can impact blood sugar levels. Dr. Carman points out that even one hour less of sleep can affect gastrointestinal hormones involved in blood sugar regulation. Aim for 7-9 hours of quality sleep, establish a regular sleep schedule, and address sleep disorders like sleep apnea.
Chronic stress can increase blood sugar levels. Incorporate relaxation techniques such as meditation, deep-breathing exercises, or yoga into your routine. Engaging in hobbies and activities you enjoy and seeking support from friends, family, or professionals can also help manage stress effectively.
7. Focus on Gut Health with Probiotics
“These bacteria play a huge, huge role… If there’s a way to always look at the diet first because these bacteria really play a huge, huge, huge role.” – Dr. Kristina Carman
The gut microbiome significantly influences blood sugar regulation and insulin sensitivity. Incorporating probiotics and fermented foods can enhance gut health.
Key Probiotic: Akkermansia Muciniphila
Benefits:
- Enhances gut lining integrity
- Improves glucose tolerance
- Supports weight management and metabolic health
Sources:
- Yogurt with live cultures
- Fermented foods like kefir, sauerkraut, and kimchi
- Probiotic supplements containing Akkermansia
8. Incorporate Whole Grains, Nuts, and Seeds
“Looking at whole grains, particularly things like black rice and quinoa and buckwheat… can be really supportive.” – Dr. Kristina Carman
Whole grains, nuts, and seeds are rich in fiber, which slows glucose absorption and improves blood sugar control. Examples include quinoa, buckwheat, black rice, almonds, walnuts, flaxseeds, and chia seeds. These foods also provide essential nutrients and healthy fats that support overall health.
9. Consume Flavonoid-Rich Foods
Foods rich in flavonoids have anti-inflammatory properties that can help manage Type 2 Diabetes.
Examples include:
- Berries (blueberries, strawberries)
- Green tea
- Dark chocolate (at least 70% cocoa)
These foods help reduce inflammation linked to insulin resistance and support metabolic health.
More FLCCC Diabetes Resources
Type 2 diabetes has been a big topic for FLCCC over the years. Here’s a few more resources you might find useful:
- Webinar: Poison Inc. Processed Foods and Prescription Drugs
- Protocol: I-CARE Insulin Resistance Treatment
- Guide: Eat Well – Guide to Healthy Eating
- Webinar: How Berberine Helps Manage Type 2 Diabetes
- Story: How Dr. Marik Reversed Type 2 Diabetes
Change Your Lifestyle Today!
Managing Type 2 Diabetes doesn’t have to be overwhelming. By making simple lifestyle changes—like adjusting meal times, eating mindfully, incorporating yogurt and fermented foods, using natural remedies, exercising regularly, and prioritizing sleep—you can effectively control your blood sugar levels.
“You cannot out-supplement a bad diet. We need to focus on modifying the diet first before adding probiotics because our bodies respond differently to natural sources.” – Dr. Kristina Carman
Remember, you’re not alone on this journey. With education, support from healthcare professionals, and dedication, you can manage your Type 2 Diabetes and lead a healthier life.
“With dedication and support, living a healthy life with Type 2 Diabetes is entirely achievable.”
Always consult with a healthcare professional before making significant changes to your diet or exercise routine, especially if you have underlying health conditions or are on medication.