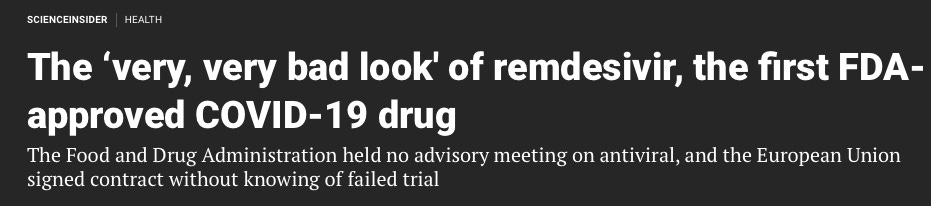
Among the most sensational and underreported stories so far this year is that Remdesivir earned more money from hospitals for treating COVID-19 in 2021 than any treatment for any other disease – despite the fact that it doesn’t work.
Vizient, the group that publishes this data, doesn’t disclose the actual dollar amounts, but rather a ranking of top drugs by sales from hospital reports. However, we know from publicly available data that Gilead earned a whopping $4.2 billion from sales of Remdesivir in the first nine months of 2021. This means hospitals probably spent over $5 billion dollars last year on a drug that is at best useless against Covid-19, and at worst dangerous to patients who receive it. And according to Vizient’s projections, hospitals could continue to blow out the spending on Remdesivir and keep it in the top spot through mid-2023.
In his article for RealClearMarkets, Dr. Pierre Kory provides a sober assessment of this blockbuster drug:
“Despite some initial indication that Remdesivir might slightly reduce recovery time, the World Health Organization conducted a large-scale analysis that found it “had little or no effect on hospitalized patients with COVID-19, as indicated by overall mortality, initiation of ventilation, and duration of hospital stay.” Unsurprisingly, the WHO recommended against using this drug to treat Covid-19 in November 2020 (and still does).
At worst, however, Remdesivir is harmful. A subsequent analysis of the agency’s safety database found it likely caused kidney failure, and when independent trials (those not sponsored by a pharmaceutical company) are analyzed alone, there is a clear statistical trend to harm. WHO also warns that the drug may be associated with an increased reporting of liver problems.”
All of this begs the obvious question: How is it possible that U.S. hospitals maxed out their spending on an ineffective and potentially dangerous drug that is scarcely used throughout the world?
Sadly, it’s because our drug approval system is broken – and has been for quite some time. During the pandemic, U.S. regulators have given speedy review and approval for expensive new drugs produced by our pharmaceutical industry, which have marginal benefit and may be dangerous. And they’ve ignored well-known, safe, cheap, generic drugs that in some cases have far more independent data supporting their clinical benefit against Covid-19.
Dr. Kory brings the receipts:
“Look at this chart created by an independent researcher that displays the efficacy of all drugs and compounds that have been studied against COVID-19. The ones circled in red are the only medicines that have received FDA Emergency Use Authorization (EUA is essentially fast-track approval) in the U.S. Each authorized medicine commands an exorbitant price while all the low-cost, effective drugs remain unauthorized for treatment of Covid-19. It would be an astonishing coincidence if the price tags were unrelated to their FDA status.
Moreover, Remdesivir was approved based on a single, small trial with questionable results. This should never be the basis for approving a medicine for mass use – even during a public health emergency. The same thing has happened with monoclonal antibodies, Pfizer and Merck’s antiviral pills, and, of course, the Covid-19 vaccines.
Even more troubling are reports that the FDA did not consult the Antimicrobial Drugs Advisory Committee in granting Remdesivir’s EUA. But the committee consists of outside experts that the FDA has at the ready precisely to weigh in on antiviral drug issues. It boggles the mind that the agency would authorize a drug without even consulting the very body that is supposed to advise it on such issues.

Compare these lightning-fast and flimsy approvals to the non-existent government response to mounting data that fluvoxamine is effective against COVID-19. The Journal of the American Medical Association and the Lancet have each published large, randomized trials to this effect, with the latter showing fluvoxamine reduced COVID-19 hospitalizations by two-thirds and deaths by over 90 percent.
The NIH review of the fluvoxamine studies unsurprisingly takes great care to highlight potential study biases while dismissing the importance of the outcome benefits found, while ignoring the limited benefit and far more glaring flaws in the Remdesivir study. Fluvoxamine already has full FDA approval. It is safe and inexpensive (a pill costs about $1). Given what we are seeing with the patented and expensive drugs like Remdesivir (a course costs about $2,400), perhaps fluvoxamine’s small price tag is the problem.
As if this all weren’t dispiriting enough, we have undoubtedly spent so much on Remdesivir because hospitals have a major financial incentive to administer it. The Centers for Medicare & Medicaid Services established a system that provides a 20% bonus to each hospital’s bill to encourage them to use Remdesivir and other EUA approved high cost, patented medications.”
We can’t change this corrupt system overnight. But we can take steps to balance the influence of pharmaceutical powerhouses on the drug review process. One way to accomplish this is to create an independent, well-funded government body dedicated to conducting fairly designed and transparent research studies of repurposed generic treatments. Another is for physicians to stop blindly following ineffective hospital protocols and treating patients with useless and potentially dangerous drugs. They must take a more active role in the practice of medicine by studying and understanding the growing body of evidence for repurposed, generic treatments.
As Kory notes, “If more physicians stood up against bad guidance based on a corrupt system, we could reclaim some of our autonomy and marshal the freedoms we once enjoyed, treating patients as we deem appropriate. That’s how physicians practiced for centuries before we were sold out to the highest bidder.”
You can read the piece in its entirety at RealClearMarkets.
More on: Big Pharma | COVID Policy | Dr. Pierre Kory | Op-ed | Real Clear Markets | Remdesivir | substack