Speakers: Dr. Yusuf (JP) Saleeby, Dr. Tom Moorcroft
Diagnosing Lyme Disease: Is it Lyme, Long COVID, or Long Vax?
Diagnosing Lyme disease has always been a complex challenge. For many patients, a tick bite is detected, antibiotics are administered, and they recover. However, studies reveal that around 20% of those who contract Lyme experience persistent symptoms for years, evading diagnosis and proper treatment.
The emergence of chronic illnesses like long COVID and long vax has only made diagnosing Lyme more difficult. Yet, for a select group of doctors experienced in treating Lyme and other chronic conditions, the overlap is clear:
“Because we are Lyme literate, we’re also COVID literate, so there’s a great overlap. There’s a lot of commonality, common side effects, symptoms, and signs from COVID illness, Lyme illness, and mold illness. They sometimes mimic each other and can be very difficult to differentiate, as some folks come in with multiple issues.” – Dr. JP Saleeby
This intricate overlap makes diagnosing Lyme even more challenging, especially given the range of other infectious diseases with similar signs and symptoms. The result? Patients remain chronically ill without understanding why, and traditional treatments fall short.
But does it have to be this way? According to FLCCC Senior Fellow Dr. JP Saleeby and Lyme expert Dr. Tom Moorcroft, the answer is no!
This webinar is essential for you if:
- You know anyone with a history of Lyme.
- You know anyone with unexplained chronic illness.
- You are a doctor striving to help your patients.
- You are curious about complex medical conditions.
Join us for this enlightening webinar and be astounded by the wealth of clinical experience our guests bring to the table. As respected leaders in their field, they offer invaluable insights you won’t want to miss.
Meet Our Lyme Disease Experts
The webinar above features two doctors who are incredibly accomplished in the diagnosis of Lyme disease and other complex chronic illnesses.
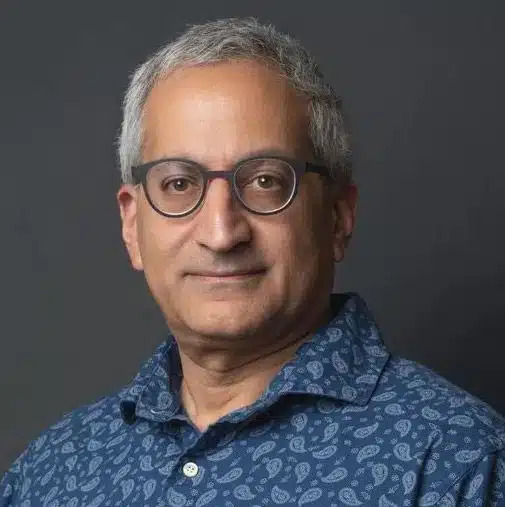
Dr. JP Saleeby, FLCCC Senior Fellow, Functional and Integrative Medicine
Dr. JP Saleeby is the medical director and founder of Carolina Holistic Medicine, a healthcare center focused on functional and integrative medicine with two locations in South Carolina. The center extends its services nationwide and internationally, serving a diverse clientele. Dr. Saleeby’s team includes highly trained advanced providers, such as nurse practitioners and physician assistants, whose education he has advanced through the Priority Health Academy.
This academy, founded by Dr. Saleeby in 2016, aims to educate practitioners and assist them in establishing independent, non-hospital, non-system-based clinics. You can keep up with Dr. Saleeby on his active Substack page.
Dr. Tom Moorcroft
Dr. Tom Moorcroft is a seasoned healthcare professional specializing in Lyme disease and chronic illness treatment. With mentorship from renowned experts like Dr. Richard Horowitz and Dr. Charles Ray Jones, he emphasizes clinical diagnosis supported by lab data. Dr. Moorcroft’s holistic approach considers environmental toxins and overall patient well-being.
He shares his expertise through his YouTube channel, Origins of Health, offering comprehensive health series and healing sessions, and The Lyme Insider podcast, where he discusses chronic illness with leading experts. His website provides free resources and educational materials to support patients and practitioners in their health journeys.
Why Diagnosing Lyme Disease is So Difficult
The Centers for Disease Control (CDC) estimate there are around 476,000 people who contract Lyme disease every year. With that many patients in the system, you’d expect the condition to be well understood and well managed by doctors.
According to Dr. Saleeby, diagnosing and treating Lyme is a challenging process:
“Well, I’ll start off by saying a lot of folks are okay with the belief that there’s the acute Lyme. They see the bullseye, they get their 21 days of doxycycline, and they think that’s it, one and done. So I think the misconception is that you’re easy to diagnose and easy to treat, and it’s actually the polar opposite. It’s very, very difficult to diagnose with serology tests.”
How Do Patients Get Lyme Disease?
Most people think that Lyme disease comes only from tick bites. Though they are a key factor, tick bites aren’t the only thing that can cause Lyme disease. Here are some other potential methods of transmission:
- Congenital (via placenta): It is possible for Lyme disease to be passed from mother to child during pregnancy.
- Unclear Routes:
- Mosquitoes and Fleas (any arthropod): There is some uncertainty about whether other arthropods can transmit Lyme disease.
- Sexual Transmission: The possibility of sexual transmission is still unclear and under investigation.
- No Evidence of Transmission via Blood Supply: Currently, there is no evidence to suggest that Lyme disease can be transmitted through blood transfusions.
- Babesia and Anaplasma: Other tick-borne diseases like Babesia and Anaplasma have been reported to be transmitted through blood transfusions.
Additional Points:
- Many people are unaware they have been bitten by a tick.
- Approximately 30% of those infected will show the “bull’s eye lesion.”
- Most reference lab tests may miss or mislead in diagnosing Lyme disease.
Misconceptions About The Bullseye Rash
Most people know that Lyme disease is caused by a tick bite. And most people have heard that when an infected tick bites, it leaves behind a distinct “bullseye” rash.
But, as Dr. Moorcroft points out, that rash is not the dead-giveaway we think it is, “We’re looking for a rash that only occurs 30-50% of the time“. Have a look at this image – these are all examples of what tick bites can look like in Lyme patients.
The Challenge of Testing and Diagnosis for Lyme Disease
Testing for Lyme disease is challenging, often resulting in false negatives. Dr. Saleeby highlights, “you can have a negative blood test, and you can still have Lyme disease,” meaning a negative result doesn’t rule out the disease. Many patients remain undiagnosed for years, enduring persistent symptoms without explanation.
Diagnosing Lyme is typically a “clinical diagnosis,” relying more on the doctor’s evaluation of symptoms and medical history than on lab tests alone. Dr. Saleeby notes, “If you have sick B cells that are not producing antibodies, you’re not going to have those on your test,” emphasizing the limitations of blood tests. Immune dysfunction can prevent detectable antibodies, leading to false negatives.
Instead of depending solely on lab tests, Dr. Saleeby advocates for a multi-faceted approach. The Horowitz Lyme-MSIDS Questionnaire, for instance, evaluates symptoms and risk factors for Lyme and other tick-borne illnesses, providing a broader understanding and improving diagnostic accuracy.
What Are The Classic Symptoms of Lyme?
Lyme disease often begins with a set of symptoms that are commonly referred to as “the summer flu.” During the acute phase, patients may experience:
- Fever
- Chills
- Headache
- Fatigue
- Muscle and joint aches
- Swollen lymph nodes
- Rash (erythema migrans)
What is Lyme Disease Often Confused With?
Lyme disease often mimics other conditions, making accurate diagnosis challenging. Dr. Moorcroft highlights this issue:
“People are asking about fibromyalgia and POTS, dysautonomia, and these conditions can often be confused with Lyme.”
Additionally, there are other factors that can complicate the diagnosis. Dr. Saleeby points out:
“There are other things we have to consider that are not always top of mind, like mold illness, heavy metals, and other environmental factors.”
Lyme disease can also have severe neuropsychiatric manifestations. Dr. Saleeby shares:
“People who suffer from Lyme or tick-borne illness, 50% of them have some type of neuropsychiatric manifestation. I have seen frankly psychotic people walking into my office who’ve just been discharged from a mental hospital, all jacked up on Thorazine and Haldol. And they diagnose with Lyme and they’re treated for Lyme and they get better. So that’s a very important thing. If you have little children and adolescents with behavioral problems, you’ve got to think Lyme could be in there.”
How Has Long COVID & Long Vax Complicated Lyme Diagnosis Further?
Dr. Saleeby discusses how the overlap between long COVID, long vax, and Lyme disease complicates diagnosis:
“I have lots of new patients coming in saying, ‘Hey, I’ve been suffering from long COVID for the last year and I can’t shake it.’ They’ve tried all sorts of protocols and they’re not improving. One of the first things I do is look for stealth infections. I check them for Lyme, Epstein-Barr, Bartonella, mold toxicity, heavy metals, and even now, electromagnetic fields seem to pickle people and prevent them from healing like they should. So when somebody has plateaued out, you have to look at underlying stealth infections and ensure all their nutrients are met. You can’t just be laser-focused on the spike and nothing else because those folks won’t get better.”
The Future of Lyme Disease
Diagnosing Lyme disease is a complex and challenging process, further complicated by the emergence of long COVID and long vax. Misdiagnosis and persistent symptoms leave many patients suffering without clear answers. However, experts like Dr. Saleeby and Dr. Moorcroft emphasize the importance of a comprehensive, multi-faceted approach to diagnosis and treatment, considering various symptoms, environmental factors, and potential co-infections.
Enhancing our knowledge and refining diagnostic methods offers hope for more effective management and treatment of Lyme disease and its associated conditions. For insight into successful treatments, watch Sophia’s patient success story, which details how hyperthermia therapy helped achieve her remission.