My husband Fred and I had dinner recently at the home of good friends, Brad and Jodie (not their real names). I met Jodie about twenty-five years ago through our kids, who were schoolmates.
Over time, Jodie and I found that we shared many interests and passions—including support of charitable organizations, social justice advocacy, education, religious life, good food, and above all, left-leaning politics. (In 2020, I was—and still am—all in for Pete Buttigieg. She preferred a different democratic candidate. Still, it felt like we were aligned in our bigger vision of salvaging democracy.)
The lively conversation we were having that evening took a somewhat different tone when Brad looked up at Fred and asked, “So, tell me about ivermectin.”
Jodie was just coming back into the dining room, having taken the dinner dishes into the kitchen.
“Oh, are we talking about ivermectin? Good! I want to know more about this,” she said, sitting down and waiting for Fred to begin answering Brad’s question.
Fred and I looked at each other, because we knew exactly why Brad was asking. Yes, he really wanted to know what Fred, a physician, knew about ivermectin—a thirty-five-year-old workhorse of a drug, ranked by the WHO as safer than an aspirin; a drug that won its developers the Nobel Prize in Medicine in 2015; and a medicine that has eradicated parasitic pandemics and saved millions of lives in low-income and developing countries since 1987. He truly wanted to know if it actually worked, as many scientists, doctors and researchers have claimed, to treat every stage of covid-19 illness—from prevention to severe disease.
But more than that, we knew that what he really wanted to know was, “Fred, why were you dragged so mercilessly through the mud in the local and national media last month after you prescribed ivermectin for a dying patient whose wife went to court to compel the hospital to give it to him?”
Fred (and I) welcomed the opportunity to tell Brad and Jodie the whole story. Actually, we were excited. Since Fred’s rather infamous turn this fall in the media spotlight, regular phone calls and texts from friends stopped for awhile. I don’t think people knew what to say to us. They had seen or read what major media outlets were saying about Fred, and they were shocked. So were (are) we.
For the next forty-five minutes, the story unfolded. They asked questions. We answered. I found myself refreshing my wine glass a few too many times as the whole story was revealed. With each passing minute, I became aware of a feeling of complete catharsis—a kind of calm that washed over me as I sat there with Fred…being heard at last by smart, well-read, reasoned friends who took in every word.

The account that follows is a summary of the story we told to Brad and Jodie. I would ask that you really “listen” as you read it. I don’t expect that every reader will instantly jump on board with what is presented here. But just know that what follows is the tough-to-take truth of what occurred. This is the story that many people would rather you did not hear.
Above all else, perhaps this story—now more of a “cautionary tale”—will help you see that the astonishing loss of life this pandemic has caused—and is still causing—was mostly unnecessary. Those innocent lives can never be reclaimed.
But the monstrous reasons why they died can be exposed.
My husband is Dr. Fred Wagshul—a Dayton, Ohio area pulmonologist/critical care specialist with an unblemished 35-year career spent saving thousands of lives. He is also one of the eight founding physicians of the Front Line COVID-19 Critical Care Alliance (FLCCC), now a 501(c)(3) non-profit organization. The now globally renowned FLCCC came together in March of 2020 to develop protocols to save patients dying of COVID-19.
The corrupt defamation of Fred (and many, many other doctors) by the media for his use of ivermectin to save his patients easily rose to the level of slander and libel…for which we are currently studying legal remedies. But to understand how we got here, the backstory is a necessary preface…
When the FLCCC was formed and Fred became one of its founding doctors, I began volunteering to assist with public relations and marketing. It started when Dr. Paul Marik (who is the co-founder, co-chief medical officer, and intellectual leader of the FLCCC) reached out to me through a mutual friend to ask if I could help him, along with several other doctors who he had enlisted, to gain the attention of then New York Governor Andrew Cuomo, then President Trump, or any other federally elected official or appointee who could help. Dr. Marik—who is the most highly published critical care physician in the United States—wanted to urgently let them know that he had developed a protocol using corticosteroids that could save the majority of critically ill covid-19 patients that were crashing into the nation’s ICUs.
The FLCCC’s tiny team soon included eight like-minded physicians, former CBS Consumer Affairs Correspondent Betsy Ashton, and me—a career marketing and communications executive. Working with Dr. Marik, and Drs. Pierre Kory, Joseph Varon, Umberto Meduri, Jose Iglesias, Keith Berkowitz, Howard Kornfeld, and Fred, Betsy and I quickly drafted a press release to send to every news organization we could possibly reach.
But the World Health Organization (WHO) had already issued a strong recommendation against the use of corticosteroids for critical covid-19 illness. So despite repeated pleas to the WHO, the CDC, the NIH, the FDA, and the general public, no one responded to Dr. Marik or the FLCCC physicians—who together have published several medical textbooks and over 2,000 papers in medical journals around the world.
Repeated claims by the FLCCC that covid-19 was a “steroid responsive disease” went unheeded for months while thousands continued to die everyday—unnecessarily. Mortality rates from covid-19 in the nation’s hospitals ranged from averages of anywhere from 25 to 80 percent. The hospital ICUs where the FLCCC doctors worked were experiencing mortality rates of 4 to 8 percent. We conveyed this information to America’s public health agencies. To CNN, The New York Times, The Wall Street Journal, The Washington Post, and many more.
Wicked, wicked silence.
It was only after Oxford University in the UK published its “Recovery” trial in late June, 2020, demonstrating the ability of corticosteroids to rescue critically ill patients, that the WHO issued a new recommendation that corticosteroids should be used for covid-19.
Well now. Whaddaya know about that…
The WHO’s recommendation for the use of corticosteroids—though lethal in its tardiness—was a sort of victory for the FLCCC. It must be mentioned here, however, that the FLCCC critical care team argues (still) that the steroid studied by Oxford University—dexamethasone—was the wrong corticosteroid, tested at the wrong dose; yet even that drug helped to recover patients in the trial. The FLCCC maintains that methylprednisolone is the superior component and should be given at a higher dose to critically ill covid-19 patients. More people could (and still can) be saved if hospitals would switch to methylprednisolone at the dosing in the FLCCC’s MATH+ Protocol. (MATH+ is the acronym for the protocol that includes Methylprednisolone, Ascorbic Acid, Thiamine, and Heparin, plus several additional co-interventions.)
In the summer of 2020, with covid cases still rising, the FLCCC physicians began to research components and combinations of therapies that could aid in the prevention and early treatment of covid-19. That was the logical next front for the FLCCC doctors. If powerful interventions could be found to deter the virus, then the number of people getting sick enough to go into the ICU would plummet, and far fewer would die.
During that summer, researchers and scientists around the world were also racing to develop covid-19 vaccines. However, the availability of vaccines getting into arms was months away, so Dr. Marik, Dr. Kory and the FLCCC critical care team shifted into high gear. They began to pore over dozens of research papers that were coming in from around the world on newly identified therapeutic interventions that were showing promise in their ability to stop the progression of early covid-19—before the virus had an opportunity to advance to critical disease.
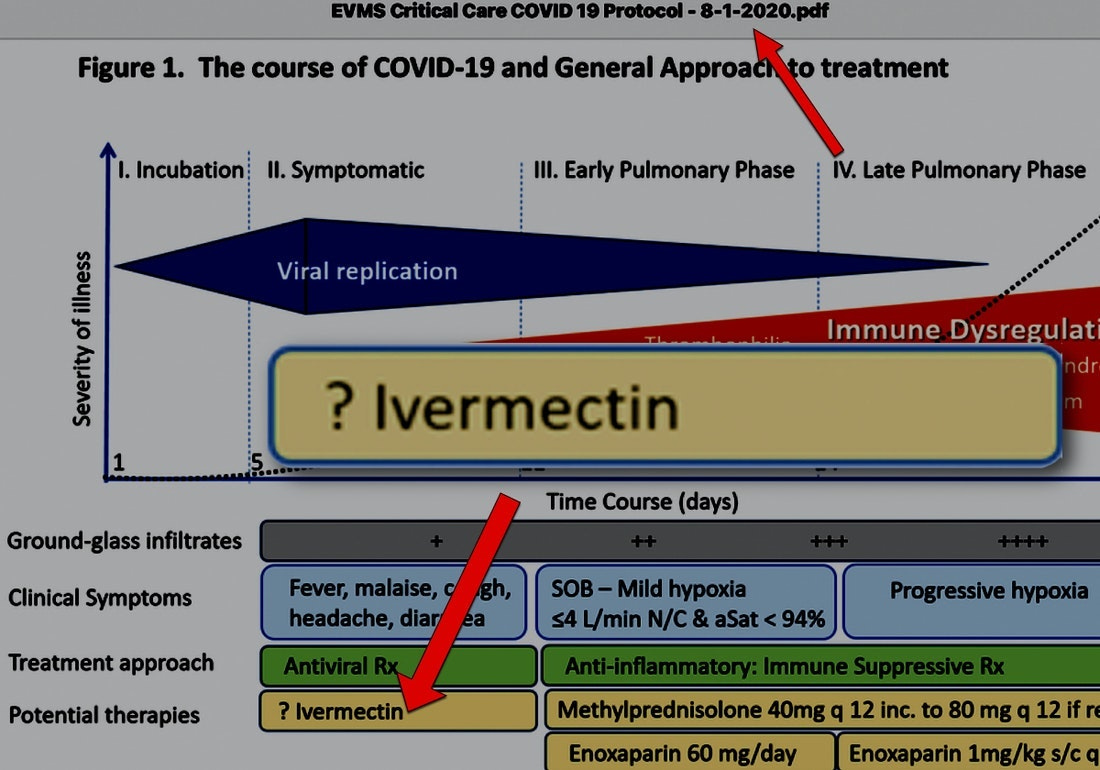
On August 1, 2020, Dr. Marik placed “ivermectin”—with a single question mark before it (?ivermectin)—on the FLCCC’s website as part of a graph explaining the progression of covid-19 disease and the general course of treatment. It marked the time when studies on ivermectin were emerging from countries around the world, demonstrating ivermectin’s effect on covid-19 illness. While Dr. Marik was intrigued enough to place it on the FLCCC website as a therapeutic “to watch,” he still wanted—and needed—more corroborating scientific data before he would be ready to recommend its use. For him—and for all of the FLCCC physicians—it’s the science that rules.
The question mark remained before ivermectin as a “potential therapy” on his graph for a few more months—until November 1, 2020. That’s when Dr. Marik, along with Dr. Kory and the other FLCCC physicians became 100 percent convinced that the rapidly emerging science conveyed a clear “data signal” pointing to ivermectin’s reproducible efficacy in both preventing and treating covid-19. Their deep review of all of the incoming data led the FLCCC to develop the I-Mask+ Protocol for covid-19. (“I-Mask+” is ivermectin, mask wearing, and other social mitigation practices, along with several additional components including vitamin C, vitamin D, melatonin, quercetin, zinc, and more.)
During a live December 4, 2020 press conference in Houston, the FLCCC doctors called for the protocol’s urgent adoption by global health authorities—who could subsequently issue immediate guidance for prescribing physicians around the world. They also emphasized that ivermectin—which won its developers the Nobel Prize in Medicine in 2015—was inexpensive, exceedingly safe, off-patent, and widely available globally. “With continued mask-wearing, social distancing and hand-washing, it can get this nation back to work,” they said. “That can happen even before the widespread distribution of the vaccines…which we are all awaiting.”
Wait. Hold on. What was that? Ears perked up.
Alarm bells began to peel.
So if the FLCCC was saying that ivermectin, along with the other components in the protocol, could prevent and treat covid-19, did that mean that they were saying that the protocol would obviate the need for vaccines?
No.
They were saying that people did not have to die while awaiting their turn to get the vaccine. It meant that people in countries without access to the vaccine also did not have to die. Neither did people for whom the vaccines were contraindicated…or those with religious or personal reasons for choosing not to receive the injection.
It meant that it would take more than one way to conquer covid. Vaccines, mitigation strategies, along with a standard of care for prevention and early treatment, were all essential in the war against covid-19.
The protocol was neither conceived nor offered as an anti-vaccine regimen. It was an anti-dying prescription. It was a covid-19 safety net.
And it worked. Well. Very well.
But it soon became evident that Big Pharma and the nation’s public health agencies did not quite see it that way. Why? Because ivermectin is cheap, so it is unprofitable. It is a super-safe, powerhouse drug and its emergence as a proven, lifesaving therapy for covid-19 caused the industry to conjure visions of mega-profits from the vaccines and other novel covid drugs streaming in white-capped torrents down an insatiable drain.
That’s why they viewed the I-MASK+ Protocol as such a fierce threat to the vaccines—in which they had invested trillions of dollars. They believed that if the lifesaving message of the I-MASK+ Protocol was permitted to be disseminated without challenge, then somehow, the vaccines and the money that would be made from them would simply evaporate.
A thorough delineation here of the massive, coordinated campaign that ensued to malign ivermectin—including its high safety profile and its ability to thwart the virus—is unnecessary, given how ubiquitous its manifestations have become worldwide. But a few are worth mentioning for context.
- Merck, the drug company that held the patent on ivermectin until 1996, issued a statement questioning the safety of its own drug for covid-19—without supporting scientific evidence. They neglected to remind the world that ivermectin had been safely eradicating pandemics for nearly forty years. Oh, and they were just days away from announcing that they were developing an antiviral pill, with modes of action similar to ivermectin, for covid-19. Not at all subtle, Merck. (Recently, the drug Merck was developing, Molnupiravir, has been shown to have far less efficacy than earlier reported by the company. Additionally, questions remain about its safety, including its reported mutagenic properties that some physicians and scientists say are of concern for sexually active men or women during childbearing years.)
- In early 2021, the World Health Organization refused to consider all of the trials showing ivermectin’s effectiveness before issuing its non-recommendation of ivermectin. They claimed that “more studies are needed.” More than the sixty trials they already had? Many of them randomized controlled trials (RCTs). Most peer-reviewed. All they had to do was consider the trials they had inexplicably failed to include in formulating their recommendation. Why did they refuse to do that?
- The COVID-19 Treatment Panel of the National Institutes of Health issued only a “neutral” stance on ivermectin after the FLCCC physicians met with them and provided them with all of the evidence from the studies—and shared the astounding statistics on all the lives it was saving. Could it be that only the incremental “neutral” stance was issued because eight of the panel members were involved either as consultants or held positions on Merck’s advisory board? Because other panel members served on the board or as consultants to Gilead Life Sciences—makers of Remdesivir? (Remdesivir remains a $3K-per-dose first-line treatment in the nation’s hospitals despite numerous studies reporting that it provides no clinical benefit.) Were other panel members associated professionally with GlaxoSmithKline, Pfizer, Regeneron, Janssen, Eli Lilly, and Bristol Myers Squibb compromised in their votes on the recommendation for ivermectin?
The coordinated attack by Big Pharma, major media, and government agencies was meant to leave ivermectin beaten, bruised, and whimpering in the shadows, zapped of its power to do what it knew it could: Save lives. The campaign shamed and mocked the FLCCC, the British Ivermectin Recommendation Development Group (BiRD) from the UK, along with other like-minded organizations and any physician, or healthcare provider who would dare pen a prescription for the drug they had labored so hard to disgrace.
The campaign seemed to be exceedingly fond of saying again and again that “ivermectin is not approved for the treatment of covid-19.” So, yes, that is technically true. But like hundreds of other FDA-approved drugs, ivermectin could be prescribed “off-label” for covid-19. Like aspirin is prescribed off-label for esophageal cancer, colorectal cancer, peripheral vascular disease, Kawasaki disease, hypertension, in-vitro fertilization, and preeclampsia. Like Viagra is prescribed for pulmonary hypertension and congestive heart failure. Like Atorvastin (a statin used for cholesterol control) is prescribed for rheumatoid arthritis, prevention of atrial fibrillation, diabetic retinopathy, and chronic heart failure. Like that. Chances are you’ve heard no hue and cry for those drugs to be kicked to the curb. Then again, they can’t do what ivermectin can do (and is doing, in the countries where it’s in widespread use) to bring the coronavirus to its knees.
The assault on ivermectin was debilitating. Its thorn-tipped tentacles choked off the FLCCC’s ability to help people learn how to save themselves and their loved ones from COVID. Soon, the FLCCC was de-platformed on LinkedIn, Vimeo, and Medium. YouTube removed most of the FLCCC’s videos. Teespring, which hosted the FLCCC’s online support store, shut the store down last summer with no notice. PRWeb/PRNewswire told the FLCCC they could no longer use their services to distribute press releases. PayPal, the platform used by the FLCCC to receive donations, removed the FLCCC as a client. Facebook and Twitter frequently locks the FLCCC out of their accounts for posting about ivermectin.
Far worse than the censorship, the jobs and medical board licenses of doctors, physician assistants, nurse practitioners and other prescribers writing for ivermectin began to be threatened…causing fewer and fewer health care providers to prescribe ivermectin for their patients. To further complicate matters, pharmacists in increasing numbers began to refuse to fill prescriptions for the lucky patients who had somehow managed to appear before pharmacy drop off windows with their prescriptions in hand.
Meanwhile, the scientific evidence demonstrating the efficacy of ivermectin continued to grow.
Study after study proved its ability to conquer covid in every phase of the disease.
In acts of sheer desperation not to fall victim to covid-19, people who had heard about the benefits of ivermectin—but could not obtain human grade ivermectin—turned to buying veterinary grade formulations—mostly horse paste, sold in farm supply stores and online. The FLCCC repeatedly tried to discourage people from using veterinary grade ivermectin by posting the names of tele-health providers around the country and pharmacies that would fill ivermectin prescriptions. But it wasn’t enough to help everyone obtain a doctor’s prescription. So people kept buying “horse-paste”—in the same way anyone dying of thirst and denied pure water would drink from a muddy creek.

Soon, a feeding frenzy erupted throughout all of major media-dom. Leading the charge was the FDA itself, tweeting in an odd “Hey pal” kind of language: “You are not a horse. You are not a cow. Seriously y’all. Stop it.” The tweet went viral. In emails obtained as the result of a FOIA request by journalists Mary Beth Pfeiffer and Linda Bonvie, FDA staffers were jubilant.
“The numbers are racking up and I laughed out loud,” said FDA’s Erica Johnson, Associate Commissioner for External Affairs.
“It’s been a fun weekend watching people say the words I wrote on TV and TikTok and such,” cooed Brad Kimberly, Director of Social Media for the FDA’s Office of External Affairs.
“That was great! Even I saw it!” exclaimed Janet Woodcock, Acting Commissioner of the FDA.
Soon, pictures and pithy memes of horses and horse paste were jockeying for position on social media, in magazines, newspapers—and on network news. Soon, the term, “horse-dewormer” was being used as a synonym for ivermectin by reporters and anchors.
It mattered not at all that epidemiological studies were showing dramatic reductions in case counts, hospitalizations and deaths in the over seventy countries around the world where ivermectin was in widespread use. The horse-party revelers did not care that most of the hospitalized patients in critical condition whose families had successfully petitioned the courts to compel the hospitals to administer ivermectin survived. And those across the U.S. who took ivermectin when they first became symptomatic and did not progress to serious illness be damned. This was all way too much fun.
And while the debauchery raged (and rages still), the reputations and livelihoods of courageous doctors, nurses and other health providers who dared to save their patients with ivermectin became collateral damage. The consequential debris—veritably strewn around the world on the wings of the internet—was left for them to pick up.
My husband was one of them. Here is what happened.
Part of the media coverage on “horse-paste” included the story of the Cincinnati, Ohio woman who filed a lawsuit in Butler County, Ohio to compel the University of Cincinnati’s West Chester Hospital to give her husband ivermectin after they told her there was nothing more they could do for him. Her husband, Jeff Smith, had been on a ventilator for about one month.
After a lengthy discussion with his wife concerning Mr. Smith’s clinical status and his medical history, Fred agreed to prescribe ivermectin to Mr. Smith—since the hospital was refusing to give him any additional therapy. The case went forward, and the judge granted the court order.
Then the media pounced.
They too called ivermectin “horse dewormer”—though it has saved millions the world over for decades since it was approved by the FDA in 1987. It is ranked one of the world’s safest medicines. It is on the WHO’s list of “Essential Medicines.”
Wrote Dr. Wagshul:
“So this is just to let you know that regardless of what the media may say, I know this medicine, as part of a multi-modal protocol that also includes vaccines, saves lives. On the day I became a physician, I swore to “first do no harm” as part of the Hippocratic Oath. My oath was not to a hospital, a city, a country, a state or to the nation. My oath was to protect my patients. I am publicly recommitting myself to that oath here. It is my hope that other physicians around the world will do the same.
It is true that after a patient has been on a ventilator for a prolonged period of time fighting the debilitating effects of COVID-19, options to recover these patients are few. But I have seen patients who’ve spent weeks on a ventilator be successfully weaned away and return home to their families—with the addition of ivermectin to the therapeutic cocktail.”
But the media was not finished with Fred—not by a long shot. For weeks, he was maligned and dogged by “journalists” wanting their chance to take a shot at him. Would they have raised their hands to lob their insults so willingly had they known (or even bothered to find out) that none of the over 1,700 patients Dr. Wagshul had put on ivermectin during the course of the pandemic had to be hospitalized? And that none had died?
Probably not. After all, careers are made on whose story rises to the top the fastest…much like hot air.
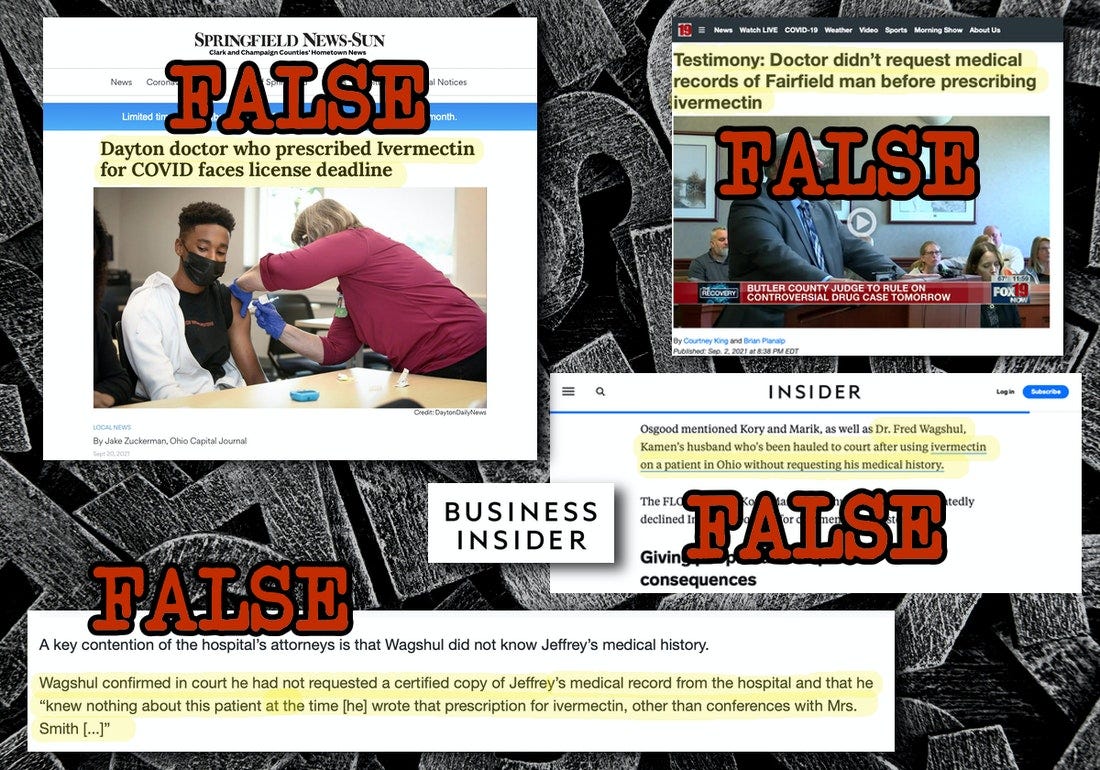
Three (of many) examples of defamatory coverage that targeted him:
- On August 31, 2021, radio talk show host Scott Sloan on Cincinnati’s WLW-AM leveled libelous, patently injurious attacks on Fred—calling him a “quack” who gave a critically ill patient “horse medicine.” Fred has been a practicing physician for over 35 years and has saved the lives of thousands of people as a pulmonologist. He does not (and has never) prescribed veterinary grade medicine to a patient.
- In a highly defamatory story on Business Insider (September 17, 2021), the writer, Hilary Brueck, said that Dr. Wagshul was “hauled into court after using ivermectin on a patient in Ohio without requesting his medical history.” This is patently false. Dr. Wagshul was never subpoenaed and volunteered to offer testimony about the efficacy of the drug during the hearing to obtain the court order. He had spoken with the wife of the ventilated patient and DID obtain his past medical history from extensive conversations with her—which included information about her husband’s history and experience on the ventilator.
- In a September 20, 2021 slanderous story by Jake Zuckerman in the Springfield News (Ohio), the headline screamed, “Dayton doctor who prescribed Ivermectin for COVID faces license deadline.” Dr. Wagshul’s license was never in jeopardy. It was a routine two-year renewal, like every other physician in the United States must also do. If Mr. Zuckerman did not know that, he has no business being a reporter anywhere.
I believe that these so-called “reporters”—and the outlets they represent—must publicly apologize to Fred. And, while we’re at it, the dozens of media companies who have allowed their employees and agents to run roughshod over Dr. Pierre Kory, Dr. Paul Marik, FLCCC physicians, Dr. Tess Lawrie, BiRD Group doctors—and all other healthcare providers around the world who dared to stand as shields in front of patients to save their lives—must be held accountable.
Lives have been lost to greed. That’s what the gun was made of. Millions and millions of innocent lives. And those who we know were party to this crime did so in broad daylight and with the assent of health policy officials worldwide who became complicit in the slaughter.
“It is written in the Talmud that ‘those who save one life save the entire world.’ Where there is life, there is hope. If we forget that as doctors, and if we throw up our hands and do not try every scientific remedy we know to save every life we can, then we are in violation of the oath we took to act in the best interest of every patient.” —Dr. Fred Wagshul
Jodie and Brad had now heard the entire story.
“Wow, this is…uh…tough to hear and to take in,” said Jodie.
“I know,” I said, sensing that the narrative she and Brad just heard probably felt like a plunge into a pool of ice. “You’re having trouble believing everything we’ve told you after only hearing for over a year now how using ivermectin for covid is nothing but right-wing quackery…right?”
“Well yes, kind of,” she said. “Wow.”
“Jodie, you know me. I am still the same Buttigieg Democrat you’ve come to know and love,” I told her, smiling. “Last time I checked, ivermectin is not on the voter rolls. It doesn’t identify as either a Republican or Democrat. It prefers to remain apolitical and save people no matter which way they pull the lever in the voting booth. It’s a drug. Like any other drug. It just wants to do what it was meant to do. And that is save lives. Lots of them.”
While I texted Jodie and Brad the website of the FLCCC, they sat quietly.
“You know, Fred and I have spent the majority of the past two years studying the science for ivermectin and all the components of the FLCCC protocols,” I told them. “Knowing what I know about the huge amount of medical evidence on the efficacy of early treatment with ivermectin and the other components in the protocol, it is incomprehensible to me that the only “guidance” that our nation’s public health agencies puts out for providers is to tell patients to stay at home until they can’t breathe and their lips turn blue, and then go to the hospital—where many end up on ventilators. There is no standard of care for early treatment. None, and that’s simply unconscionable. And until there is—or until this pandemic subsides—people will continue to die unnecessarily. I can’t believe that our country has so badly betrayed its citizens.”
I looked at my husband sitting next to me, and I don’t recall ever being as proud of him as I was that evening with Jodie and Brad. Fred knew the right thing to do for his patients, and he did it—despite the despicable, defamatory treatment he received at the bloodstained hands of the media. One by one, these lecherous reporters executed their own judgment upon Fred like good little soldiers doing what they were told to do. They knew nothing about his lifelong adherence to the highest medical ethics and his success saving the lives of his patients—many of whom come to him because even without covid, they have trouble breathing. Yes, even his patients struggling with chronic bronchitis, COPD, emphysema, and asthma were saved by Fred during the pandemic.
As we got up to leave, Brad and Jodie thanked us for telling them the tale of what we’ve been through this past twenty-one months. They have always held a lot of respect for Fred, and they asked if they could call him to discuss early treatment with ivermectin if they should come down with covid. (Fred said, “Of course.”) Meanwhile, they promised to pore through the FLCCC’s website and call him if they had any more questions.
“You’ve certainly given us a lot to think about,” said Jodie.
And so, dear reader, that is what I hope this essay has given you, too.
Stay well.